The U.S. healthcare system is currently finding itself in an increasing demand for care amid shrinking workforce capacity. Healthcare staffing shortages, once framed as “clinical challenges”, are now acknowledged as system-wide threats that strain not just patient care but also financial operations. While clinical shortages often dominate headlines, administrative functions such as Revenue Cycle Management (RCM) are equally affected. Providers simply do not have enough qualified personnel to manage billing, coding, claims follow-ups, and payer negotiations effectively, and this gap is hurting revenue integrity and operational resilience.
In this blog, we explore why staffing shortages impact RCM so acutely, how these shortages weaken revenue cycle performance, and most importantly how outsourcing RCM offers a strategic, sustainable solution for U.S. healthcare providers.
How Staffing Shortages Disrupt the Revenue Cycle
Staffing shortages in U.S. healthcare extend far beyond clinical roles and have increasingly strained revenue cycle management (RCM) functions, the critical link between care delivery and payment. The complexity of RCM work, which includes tasks like patient registration, coding, claims submission, denials follow-up, and payer reconciliation, means that even small workforce gaps can slow cash flow and increase errors. Deloitte research highlights that revenue cycle teams face high turnover and long hiring cycles, with many organizations reporting shortages in qualified RCM staff and difficulty filling these specialized roles, which can take 84 to 207 days to replace on average.
Industry data also shows that staffing shortages, both clinical and administrative, are contributing to operational burdens and financial pressure across healthcare providers. A KPMG industry update notes that staffing shortages and administrative overload are among the key drivers pushing providers toward RCM transformation and external support, with many organizations now relying more on end-to-end RCM services to navigate reimbursement complexities, optimize billing processes, and reduce denial rates. At the same time, surveys from revenue cycle professionals indicate that these staffing gaps are directly linked to slower reimbursements, rising denial rates, and longer accounts receivable cycles, underscoring why traditional hiring approaches alone are insufficient and why strategic outsourcing and technology-enabled partnerships are becoming essential.
Outsourcing RCM: A Strategic Response to Staffing Shortages
Outsourcing revenue cycle management means partnering with external experts to handle all or part of your financial operations, such as coding, billing, collections, denials management, and payer follow-up, using dedicated teams that are integrated with your systems and goals.
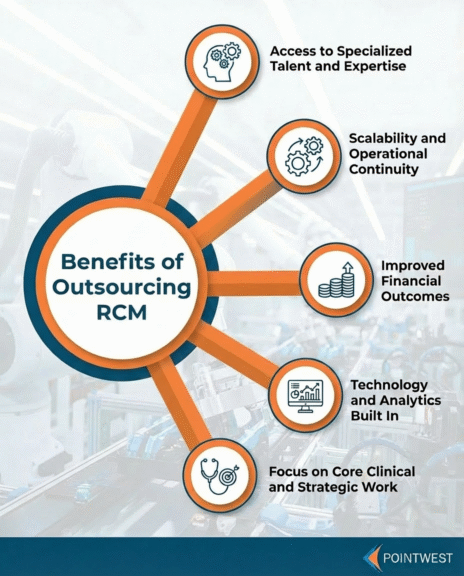
Here’s why outsourcing is emerging as a strategic solution:
- Access to Specialized Talent and Expertise
Outsourcing partners have experienced billing and coding professionals, reducing dependency on limited local labor pools. - Scalability and Operational Continuity
Outsourced teams scale capacity faster than internal hiring, especially during peaks or staff turnover. - Improved Financial Outcomes
With dedicated focus on revenue cycle functions, providers often see faster claims processing, fewer denials, and improved cash flow. - Technology and Analytics Built In
Outsourcing partners typically bring advanced RCM technology, including automation and data analytics, that smaller providers might not afford internally. - Focus on Core Clinical and Strategic Work
When revenue cycle operations are stabilized externally, internal staff can focus on patient care, quality initiatives, and strategic priorities.
Key Features Healthcare Organizations Should Look for in RCM Outsourcing
When healthcare organizations turn to RCM outsourcing to address staffing shortages, not all partners deliver the same value. The right outsourcing model goes beyond filling capacity gaps, it stabilizes revenue operations, reduces dependency on scarce talent, and improves financial predictability. The following capabilities are critical.
Integrated Coding and Billing Expertise
RCM outsourcing partners must bring deep, up-to-date expertise across medical coding, billing, and payer-specific rules. Staffing shortages often force internal teams to stretch across multiple functions, increasing the risk of coding inaccuracies, undercoding, and claim rejections. An experienced RCM partner centralizes this expertise, ensuring claims are coded correctly the first time, documentation aligns with payer requirements, and regulatory changes are continuously monitored. This reduces rework, accelerates reimbursement cycles, and protects revenue even when internal teams are understaffed.
Technology-Enabled Workflow Automation
Automation is essential when human capacity is limited. Leading RCM providers can embed workflow automation across eligibility checks, charge capture, claim submission, payment posting, and denial management. These tools reduce manual handoffs, eliminate repetitive tasks, and standardize processes that are often error-prone when handled by overburdened staff. For healthcare organizations facing persistent staffing gaps, automation ensures revenue operations continue to scale without proportional increases in headcount.
Analytics and Performance Monitoring
Staffing shortages often make it difficult for internal teams to track performance in real time. Strong RCM outsourcing partners provide embedded analytics and dashboards that surface key revenue cycle KPIs such as denial rates, days in A/R, clean claim rates, and payer turnaround times. These insights allow organizations to identify bottlenecks early, prioritize high-impact interventions, and make data-driven decisions, without relying on manual reporting from already constrained teams.
Compliance and Security Capabilities
With limited internal resources, maintaining compliance can become a risk. RCM outsourcing partners must demonstrate strong HIPAA compliance, secure data handling, and rigorous governance frameworks. This includes role-based access, audit trails, secure integrations with EHR and billing systems, and continuous compliance monitoring. For healthcare organizations under staffing pressure, these capabilities reduce regulatory exposure while ensuring revenue operations remain resilient and audit-ready.
Conclusion: Outsourcing RCM as a Competitive Advantage
Administrative burdens are rising, demand for healthcare services is increasing, and traditional hiring strategies no longer suffice.In this context, outsourcing RCM is not a stopgap, but a strategic enabler. It provides access to specialized talent, reduces operational strain, and allows providers to optimize revenue capture while refocusing internal resources on care delivery and strategic growth.
Pointwest combines deep domain knowledge with technology-enabled solutions that help healthcare organizations navigate staffing constraints, improve revenue cycle performance, and secure financial resilience. By partnering with experienced RCM experts, providers can transform their back-office operations from a bottleneck into a source of stability and growth.
About Pointwest
Pointwest is a global professional services firm enabling enterprises to transform systems into agile, interconnected business services that integrate operations, enhance digital customer experiences, and drive sustainable growth. We deliver end-to-end solutions across software modernization, quality engineering and testing, data engineering, advanced analytics, and AI/ML-driven solutions, leveraging cloud-native innovation, engineering discipline, and best practices to provide solutions that are secure, reliable, and generate measurable business value.
With experience in Healthcare, Insurance, Banking, Financial Services and Retail, we help digital-first movers advance to enterprise-ready, and regulated production, drive large-scale technology transformations, and execute digital initiatives by optimizing business processes, enhancing customer experiences, and applying fit-for-purpose technology to enable business agility while managing operational risk and compliance.
Recognized for our global delivery model and technical expertise, we partner closely with enterprises to turn strategy into execution. Pointwest is a trusted digital partner of AWS, Google, UiPath, and Tricentis, and confirmed HIPAA Compliant.
To learn more, contact us.